Prostate Cancer
 Prostate cancer is the most common non-skin cancer in men in the United States and the second leading cause of cancer death in men.
Prostate cancer is the most common non-skin cancer in men in the United States and the second leading cause of cancer death in men.
What is PSA?
Prostate-specific antigen (PSA) is a substance produced by the prostate gland. The PSA level in a man’s blood is an important marker of many prostate diseases, including prostate cancer.
When to Seek Help?
If your PSA is high for your age or is steadily rising, a biopsy may be recommended to determine if cancer or other abnormal cells are present in the prostate. Your doctor should consider other risk factors for prostate cancer such as family history, and ethnicity before recommending a biopsy.
The decision to screen is one that a man should make with his doctor following a careful discussion of the benefits and risks of screening. In men who wish to be screened, the American Urological Association (AUA) Foundation believes recommends getting a baseline PSA, along with a physical exam of the prostate known as a digital rectal exam (DRE) at age 40.
Factors to Consider About Prostate Screening
- Men who wish to be screened for prostate cancer should have both a PSA test and a DRE.
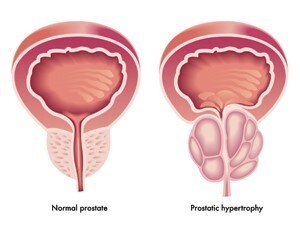
- A variety of factors can affect PSA levels and should be considered in the interpretation of results. The three most common prostate diseases—prostatitis, benign prostatic hyperplasia (BPH), and prostate cancer—may cause elevated PSA levels in the blood. Other medications, trauma or treatments (which can include a prostate biopsy or cystoscopy) to the prostate can affect PSA test results.
- PSA level in a man’s blood is generally a good predictor of the risk of prostate cancer and the extent of the cancer. Men whose PSA levels rise sharply over a short period are more likely to have prostate cancer than those who do not see significant changes in their PSA velocity.
- The decision to use PSA for the early detection of prostate cancer should be individualized. Men should be informed of the known risks and the potential benefits of early screening.
What You Should Know About Prostate Cancer Surgery
Radical prostatectomy is the removal of the entire prostate, the seminal vesicles, the tissue immediately surrounding the prostate, and some of the associated pelvic lymph nodes. Prostate cancer can be scattered throughout the prostate gland in an unpredictable way. The entire prostate must be removed to ensure that cancer cells are not left behind to continue to grow. Surgical options include the following:
What is Open Radical Prostatectomy?
There are two types of radical prostatectomies:
Retropubic Open Radical Prostatectomy is when the surgeon makes an incision through the lower abdomen that is about four inches in length. The prostate gland and the lymph nodes can be removed at the same time (generally with limited blood loss and preservation of the neurovascular bundles, which are responsible for maintaining erectile function). The surgeon is also better able to cut the tissue to remove all of the cancer.

Perineal Open Radical Prostatectomy is when the surgeon removes the prostate through an incision between the anus and the scrotum. This approach requires less time in surgery, and your recovery time may be faster. Bleeding is uncommon and because there is a smaller incision, there is generally less pain. However, the pelvic lymph nodes cannot be removed through the same incision, and this approach makes nerve-sparing difficult.
What is Robotic-Assisted Surgery?
With recent advances in minimally invasive surgery and robotic technology, the prostate gland can be removed through several 1 to 2-inch incisions in the patient’s abdomen. A surgeon operates a surgical robotic system—a device that holds surgical instruments and a camera to see inside the abdomen and remove the prostate gland through small incisions.
Advantages of this procedure are less pain, reduced blood loss and faster recovery time due to the smaller incisions. Nerve sparing is possible so sexual function is retained.
What is Laparoscopic Prostatectomy?
Laparoscopic surgery is a form of minimally-invasive surgery. The surgeon will make six 1-inch incisions, with one being slightly larger in order to extract the prostate gland from the abdomen. Through these small incisions, surgical instruments, including a camera, are inserted. The camera allows the surgeon to view inside the abdomen to perform the surgery and remove the prostate.
Laparoscopic surgery is less traumatic on patients because of the small incisions and may result in less pain and scarring, and your recovery time may be quicker. Nerve-sparing is possible with this approach and you may regain sexual function in a shorter period of time. However, you could also experience a longer period of bladder-control problems.
Short-term and Long-term Effects of Surgery
The main benefit of surgery is the removal of the entire prostate gland and your cancer. Talk to your doctor about how your surgical treatment choice will affect you in the short-term and long-term. Surgery requires anesthesia, and you may be in the hospital for one to three days and sent home with a catheter.
Long-term complications after surgery may include urinary incontinence and erectile dysfunction. If the cancer has already spread, then removing the prostate may not cure your cancer and additional treatments may be needed.
Choosing Which Surgery is Right For You
Your health history, family history, current health and the seriousness of any other disease you may have can affect how long you may live and the risks or complications associated with surgery.
Personal Preferences
Values and preferences vary. Some men want their cancer completely removed. Other men worry about how certain treatments could affect their quality of life. As a result, they may choose a treatment that avoids certain complications.
Cancer Stage and Grade
Cancer stage is an estimation of the size and location of the cancer. This shows how far the cancer has already spread. The grade indicates the aggressiveness of the cancer; that is, how quickly it may grow and spread beyond the prostate.
Life Expectancy
How long you may expect to live, rather than age, is important in choosing a treatment option. When life expectancy is longer, localized prostate cancer may cause illness and death before other diseases. Men with shorter life expectancies are often affected by other diseases before their localized prostate cancer affects their health.
Who is a Good Candidate for Radical Prostatectomy Surgery?
Prostate surgery is best if you have prostate cancer confined to the prostate, and in select cases where it has begun to spread outside of the prostate and maybe in the seminal vesicles.
Prostate cancer surgery is usually for those who are healthy enough to tolerate a major operation and have a 10-year or more life expectancy. Life expectancy is assessed by both age and health.